Testing is one of the most daunting obstacles to overcome before thousands can again pack beaches and baseball stadiums. The much-lauded gene-editing technology CRISPR is now making a bid to help fill in holes in testing regimens. Last week researchers published a study in Nature Biotechnology describing a new assay for the novel coronavirus that causes COVID-19 that uses the technique to deliver results in about 40 minutes. The work began when study co-author Charles Chiu, an infectious disease physician at the University of California, San Francisco, was researching a CRISPR-based Lyme disease test earlier this year. Then SARS-CoV-2 began its fateful journey around the globe, and he quickly shifted the research in his laboratory.
To develop the probe, Chiu and his colleagues at U.C.S.F. collaborated with researchers at Mammoth Biosciences, which was co-founded by biochemist and CRISPR co-discoverer Jennifer Doudna. The test uses different reagents than the PCR-based SARS-CoV-2 ones that are currently in use, offering a potential alternative where there are shortages of the chemicals needed to conduct the latter assays. One drawback, however, is that the new approach’s sensitivity, or ability to correctly provide positive results, is slightly lower than that of existing tests. Chiu says that it will take about two weeks to develop the CRISPR test for clinical lab use—and that a point-of-care version could be ready in as little as two to three months. Scientific American spoke with him about the technique.
[An edited transcript of the interview follows.]
How does the test work?
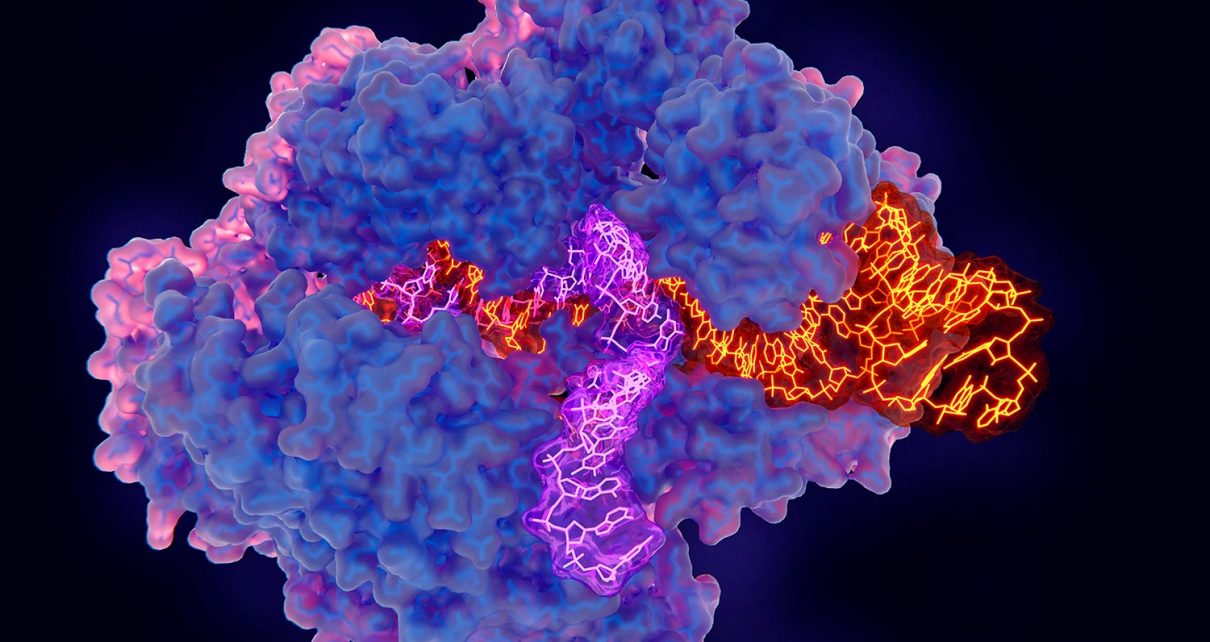
CRISPR is a technology that allows you to target any particular gene, and you can think of it almost as a molecular scissor. It can very quickly and very precisely identify a gene, or basically a portion of DNA sequence, corresponding to a virus. This is why it’s commonly thought of as a gene-editing tool. But the same technology that allows us to edit genes also allows you to detect them. In this case, we’re targeting the genes of SARS-CoV-2. We use a protein called CRISPR-Cas12. If it finds the right target, it cuts that target. And by doing so, it releases a signal.
The test detects the E (envelope) and N (nucleoprotein) genes on SARS-CoV-2. Why did you choose to target these?
There are a couple of reasons. In particular, the N gene is the gene that is most highly expressed in viral infections. In other words, it’s the most common, so it’s the easiest to detect. The second reason is that the N gene is effectively the same target that the Centers for Disease Control and Prevention’s PCR test targets. And this was the first test the Food and Drug Administration cleared for emergency use authorization (EUA), so we’re simply leveraging the fact that there’s already a test targeting that gene, which happens to be highly expressed. We selected the E gene because it’s one of the targets used by the World Health Organization. Our goal was not to reinvent the wheel but rather to use the same targets that have already been shown to be effective in detecting SARS-CoV-2.
Where does this test fit into the existing landscape of coronavirus testing—and PCR-based tests in particular?
We’re nowhere near the scale of testing that we really need in order to be confident that we can reemerge and go back to work. Although there are many different PCR tests, there’s still a need to drastically ramp up both the scale and the speed of testing. And every test that’s based on PCR uses a common set of reagents and, as a result, is subject to shortages in their availability. Our assay uses enzymes and reagents that are different than nearly all of the other tests out there, so it’s an alternative that could really ramp up testing. We also need technology that allows us to do testing in point-of-care settings: in the emergency room, in the doctor’s office or even at home. CRISPR technology provides a pathway by which we could eventually do that. It doesn’t require bulky instrumentation. And the reagents themselves are quite cheap.
Do you think CRISPR-based testing will replace PCR assays?
I don’t. It is slightly less sensitive than the PCR tests that are now commonly available. CRISPR technology still has a long way to go before we can achieve comparable sensitivity—although in principle, there’s no theoretical reason we can’t. But I do think that when the time comes, and it’s more widely adopted and optimized, it’s certainly possible, because CRISPR-based tests are faster and potentially cheaper. And in this particular test, we might be able to bypass the extraction step of converting a sample into RNA or DNA. So there’s a chance it might be able to replace conventional testing. But it’s still a new technology, and I don’t think that’s going to happen anytime soon. In the immediate term, it’s meant to be a complimentary tool.
Your approach has a 95 percent sensitivity rate. Is that good enough for mass testing?
I think it is. Patients who are infected with SARS-CoV-2 usually have the highest viral load when they initially develop symptoms. And in fact, it may even be prior to symptom onset that they may have very high viral loads. In hospitalized patients, the viral loads fluctuate over time, but generally, they go down. So when patients are minimally symptomatic, that’s when they’re incredibly infectious, and we need to find a way to break the chain of transmission. The promise of CRISPR is that it can provide a way to have cheap, decentralized testing for a large fraction of the population. Right now the need is not to detect every low-level infection, it’s to get testing implemented at a widespread scale.
Some PCR-based tests can provide results in under 15 minutes. This test takes about 40 minutes. Can you make it any faster?
In the interest of getting the test out there and maximizing its sensitivity, we chose to make it more robust. So the steps are actually longer than they need to be. Speeding up the test would involve bypassing the extraction step, as well as decreasing the reaction times. We’ve been able to decrease the detection time down to 10 minutes, so it’s definitely doable. The question is, Can you do that and still retain the same sensitivity?
Is it an inexpensive test?
Overall the test is quite inexpensive, because the reagents and enzymes can be made in bulk. The cost right now is going to be in terms of trying to manufacture the right platform. If we can package the test into a cheap, disposable cartridge, it potentially could be very cheap. The cost of reagents is just a few dollars per test. For the clinical-lab-based CRISPR test, we’re aiming for less than $1 per test, and the cost of a home-based test is under $5. The key, though, is whether [we] can manufacture [it] at high volume and high capacity and keep it cheap—and still be able to run the test in different settings outside of the laboratory.
What are the technical issues associated with scaling up testing?
The availability of reagents is one. Another simply involves the need for centralized testing. Typically, you need a molecular lab to run these instruments, so testing is limited by the number of instruments you can deploy. The Abbott ID NOW [assay], for example, is one of the few point-of-care instruments. But it runs only one sample at a time. We need to be able to run hundreds of tests at a time. And CRISPR, in addition to allowing you to do point of care because the reaction is very fast and simple, [might let you] potentially run thousands of samples a time in a clinical laboratory—and do so faster than PCR can. You can also potentially distribute it for home use. Multiplexing the CRISPR test in a point-of-care setting or at home is feasible if the test consists of a disposable cartridge containing all of the reagents you need.
Are there other places using CRISPR for infectious disease testing?
Yes, there’s a group at the Broad Institute [of the Massachusetts Institute of Technology and Harvard University] developing CRISPR-Cas13 enzymes for SARS-CoV-2 testing. And because it’s useful for diagnostics, as well as gene editing, we envision developing CRISPR to be both a diagnostic tool and a therapy that could not only detect the virus but destroy it.
What potential applications are there for using this test on emerging viruses in the future?
What’s great about this technique is that these probes can be designed on the fly, which means we can rapidly change our target. I was actually collaborating with Mammoth Biosciences on this test to develop a tick-borne Lyme disease test. Once the SARS-CoV-2 genome sequence was available, we went from having the sequence to having a functional test in two or three weeks. Eventually, we envision a point-of-care test that would be programmable for any target you wish.
Read more about the coronavirus outbreak here.