When the novel coronavirus jumped to humans in late 2019—adapting so well to its new host species that it caused a pandemic—it was beating the odds. Although scientists estimate that roughly 60 percent of known human pathogens and up to 75 percent of those associated with emerging diseases originate in animals, successful “spillover” remains exceedingly rare. According to scholars, anywhere from 260,000 to more than 1.6 million animal viruses exist in nature. Yet with slightly more than 200 viruses documented to affect humans, far less than 0.1 percent of those from other species have “ever caused a known human infection,” a 2019 PLOS Biology paper notes.
For a virus to hop from animals to people and then survive, replicate and spread efficiently among its new hosts, a number of factors must align—including ecological and viral characteristics. In recent decades, population growth, environmental disruption and the rise of industrial agriculture have altered the so-called human-animal interface. This change has led to the emergence of several zoonotic diseases, from Ebola to avian and swine influenzas and several coronaviruses.
Microbes do not make the cross-species leap in just one direction, however. Several cases of COVID-19 patients infecting pet dogs and cats have been reported. And in early April a tiger at the Bronx Zoo was confirmed to have the virus (seven of the zoo’s other big cats have since tested positive as well). Evolutionary genetic analyses indicate that during the 2002–2003 SARS outbreak, transmission between humans and small carnivores went both ways. Further, during the 2009 H1N1 influenza A pandemic, 21 countries reported infections among animals, most of which arose in the wake of the human outbreaks. In fact, since the 1980s, researchers have documented cases of humans infecting wildlife, companion animals and livestock with a wide range of pathogens, including viruses, fungi and bacteria.
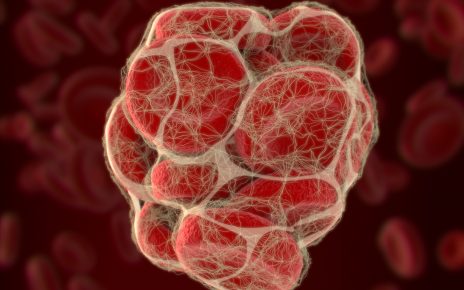
While such “reverse zoonosis” sometimes has grave, even life-threatening consequences for animals, experts say that it may also have important implications for the likelihood of future outbreaks among people. A novel virus typically emerges via mutation or an exchange of genetic material among two or more viruses when they infect a host at the same time. Although both factors play a role in viral evolution and pandemic potential, it is the latter process—known as reassortment in segmented viruses (pathogens whose genome is split into several parts) such as influenza viruses and recombination in nonsegmented ones such as coronaviruses—that makes human-to-animal zoonosis so risky.
“Any time viruses have the potential to mix and mingle with others, it can cause serious issues—especially when they can jump between animals and people in either direction,” says Casey Barton Behravesh, director of the One Health Office at the U.S. Centers for Disease Control and Prevention’s National Center for Emerging and Zoonotic Infectious Diseases.
Pigs happen to be excellent mixing vessels. The 2009 H1N1 flu virus that killed 151,700 to 575,400 people around the world in its first year of circulation spilled over from the animals. But that virus contained individual gene segments originating from four distinct sources: humans, birds, and North American and Eurasian pigs. Indeed, many of the viruses pigs harbor come from humans. In recent years, researchers have identified dozens of discrete instances all over the world in which pandemic and seasonal influenza viruses have leaped from humans to circulate among swine populations.
“We’ve had two jumps of avian viruses that have gotten into pigs. And compared to that, we’ve probably had dozens, if not hundreds, of human viruses. So the [genetic diversity of influenza in swine] is overwhelmingly of human origin,” says Martha Nelson, a scientist at the National Institutes of Health’s Fogarty International Center.
Since 2011 swine flu viruses containing human-origin genes have been associated with more than 450 zoonotic infections, mostly in agricultural fairs throughout the U.S. Although these particular strains showed only a mild capacity for interhuman transmission, the greater the genetic diversity of viruses found in a reservoir host, the more likely it is that a variant capable of spreading efficiently among people will emerge. “It’s a little like playing Russian roulette,” Nelson says. “We know these [viruses can make the species jump to] infect people. But it’s just a matter of time until one will be able to spread from human to human.”
Human-to-swine transmission of influenza has become a greater risk factor in the modern era because it presents constant opportunities for spillover in both directions. In industrial agriculture, pigs move within regions and between continents, encountering both swine and human viruses from all over the world. Often, they live in close contact with both humans and other pigs. These conditions provide viruses with plenty of chances to find the “right” mutation or new combination of genes not only to jump between species but to actively circulate. The viruses and their components bounce from humans to U.S. commercial swine to show pigs, Nelson says, until they eventually emerge as something novel in the people who spend their lives caring for the animals: farm and feedlot workers and youth livestock exhibitors.
The degree to which reverse zoonosis increases the risks of pandemics or major outbreaks more broadly remains less clear. Although the majority of emerging zoonotic diseases have originated in wildlife, not livestock or pets, Barton Behravesh notes that interactions between humans and other species are incredibly complex. “There are all sorts of features that can lead to that perfect storm that can cause a disease to switch over between animals and people,” she says. “We do know that very close contact with animals and their environment provides more opportunities for diseases to transmit between animals and people.”
So far reverse zoonosis does not appear to have shaped the trajectory of the COVID-19 pandemic. Like influenza viruses, coronaviruses are known to jump from one species to another with relative ease. SARS-CoV-2—the virus that causes COVID-19—has shown its ability to leap from humans to other animals, especially cats. Cases have been rare, however. And limited evidence suggests that cats might be able to transmit the virus to one another in close quarters, but there is currently no evidence that cats can infect humans, according to Gregg Dean, a professor and head of the department of microbiology, immunology, and pathology at Colorado State University.
Although individuals are understandably concerned about their pets’ health, Dean says that it is unlikely that companion animals will become major vectors for transmission. Even if SARS-CoV-2 were able to jump from cats back to people, the particular circumstances of feline-feline and human-feline interactions greatly reduce the likelihood that these transmissions would become a problem. Outside of feral colonies or shelters, most domestic cats are rarely in the high-density environments that result in clusters of cases being dispersed into the community. And cats are easier to test and quarantine than humans. “Our domestic cats are probably at a greater risk of getting COVID-19 from us than we will be of getting it from them,” Dean says.
Nevertheless, reexamining our assumptions about the way diseases flow will be key to preventing future pandemics. And as a result, many experts are pushing for a One Health approach that considers human health in the greater context of the well-being of animals and the environment. “We still think of humans as this clean, higher-level species and the animals being the ones with all the pathogens,” Nelson says. “But if you think about human society and our densities and our contact structures, we are incubators for pathogens.”
Read more about the coronavirus outbreak from Scientific American here. And read coverage from our international network of magazines here.