For all the mysteries that remain about the novel coronavirus and the COVID-19 disease it causes, scientists have generated an incredible amount of fine-grained knowledge in a surprisingly short time.
Thousands of different coronaviruses may inhabit the planet. Four of them are responsible for many of our common colds. Two others have already triggered alarming outbreaks of disease: in 2002 a coronavirus caused severe acute respiratory syndrome (SARS), which killed more than 770 people worldwide, and in 2012 a different strain started Middle East respiratory syndrome (MERS), taking more than 800 lives. SARS burned out within a year; MERS still lingers.
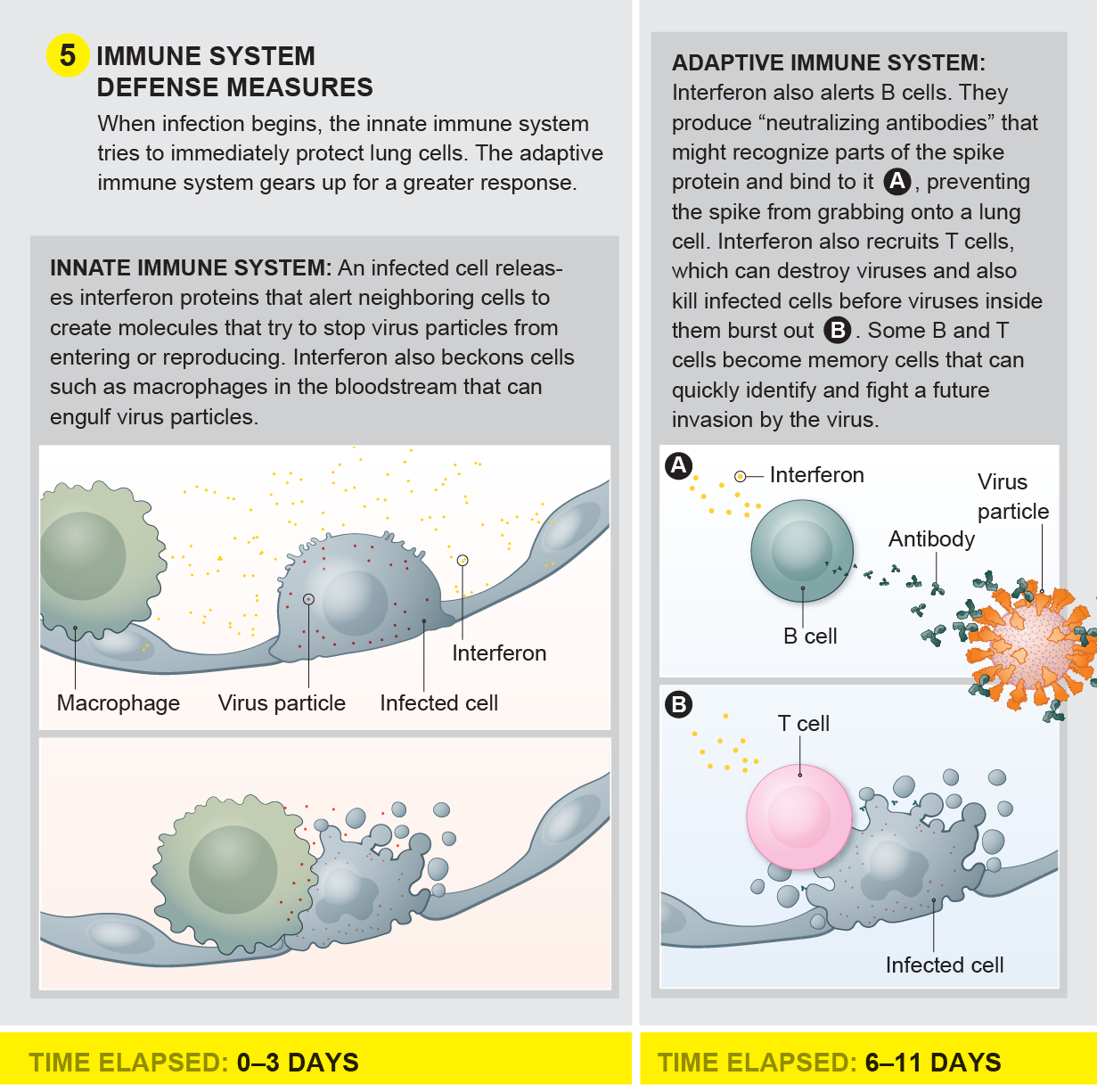
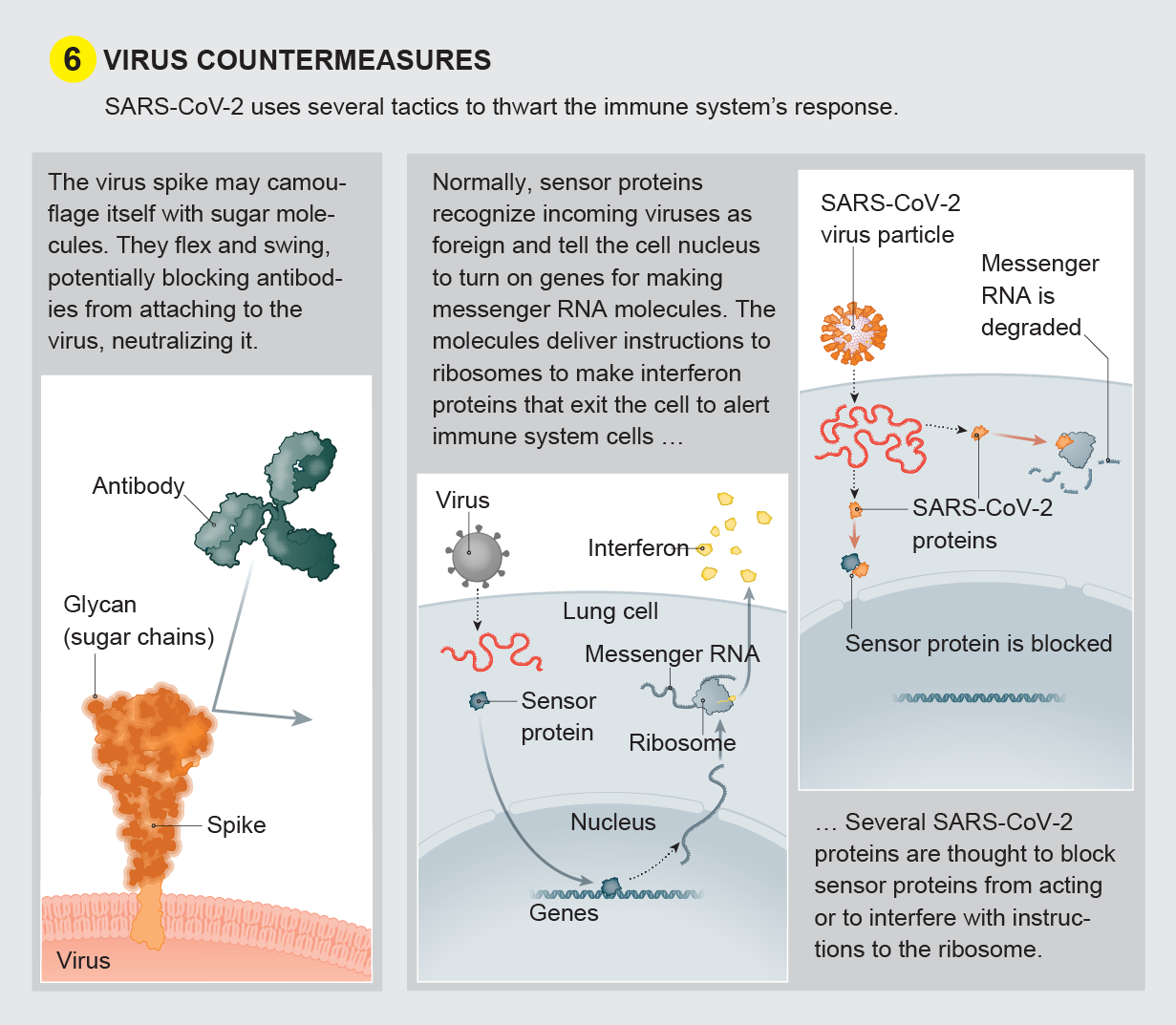
The newest coronavirus, SARS-CoV-2, has created a far deadlier pandemic in part because once it infects a person it can lie undetected for a long time. An individual who had the SARS coronavirus did not transmit it until 24 to 36 hours after displaying symptoms such as fever and dry cough; people feeling ill could be isolated before they made others sick. But people with COVID-19 can transmit the virus before they show clear symptoms. Not feeling ill, infected men and women work, commute, shop, eat out and attend parties, all the while exhaling coronavirus into the airspace of people around them. The virus can remain undetected inside the human body for so long partly because its genome produces proteins that delay our immune system from sounding an alarm. Meanwhile lung cells die as the virus secretly reproduces. When the immune system does hear the call, it can go into overdrive, suffocating the very cells it is trying to save.
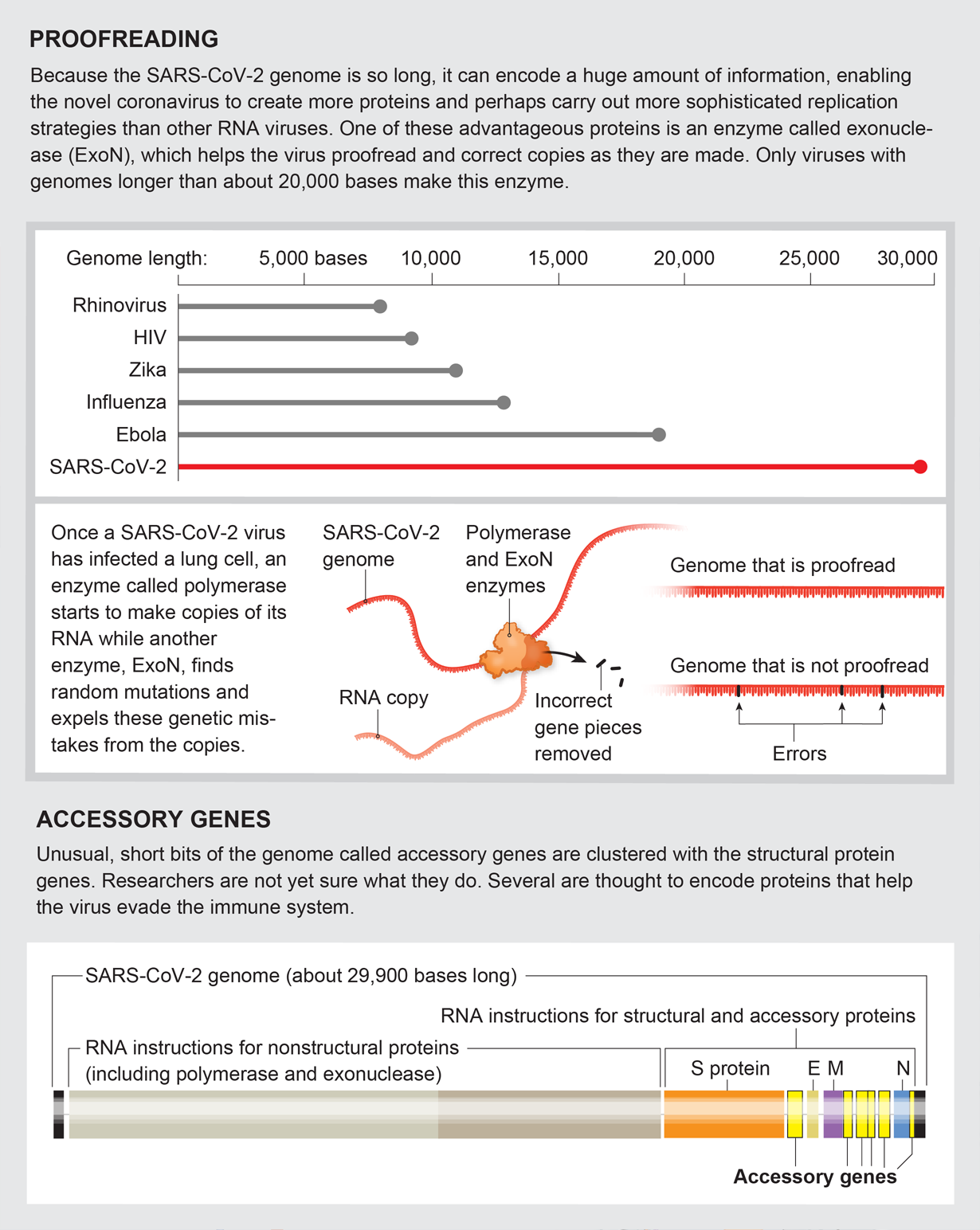
In the graphics that follow, Scientific American presents detailed explanations, current as of mid-May, into how SARS-CoV-2 sneaks inside human cells, makes copies of itself and bursts out to infiltrate many more cells, widening infection. We show how the immune system would normally attempt to neutralize virus particles and how CoV-2 can block that effort. We explain some of the virus’s surprising abilities, such as its capacity to proofread new virus copies as they are being made to prevent mutations that could destroy them. And we show how drugs and vaccines might still be able to overcome the intruders.
As virologists learn more, we will update these graphics on our Web site (www.scientificamerican.com). Greater knowledge can raise the chances for humans to prevail.
Virus Invasion and Immune Response
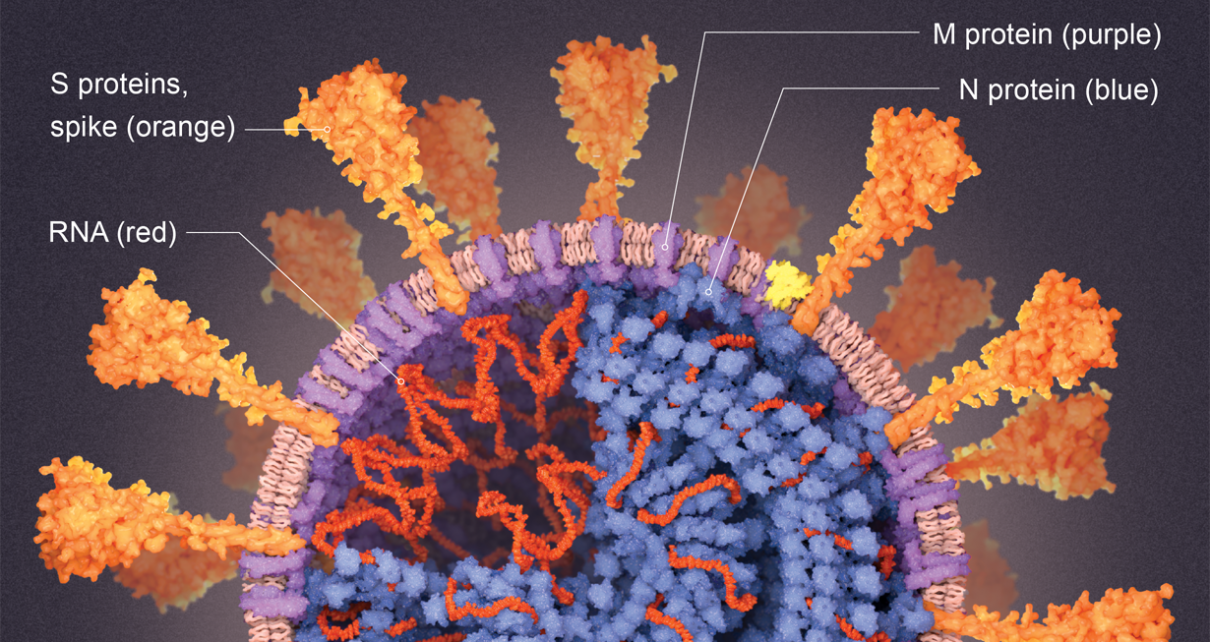
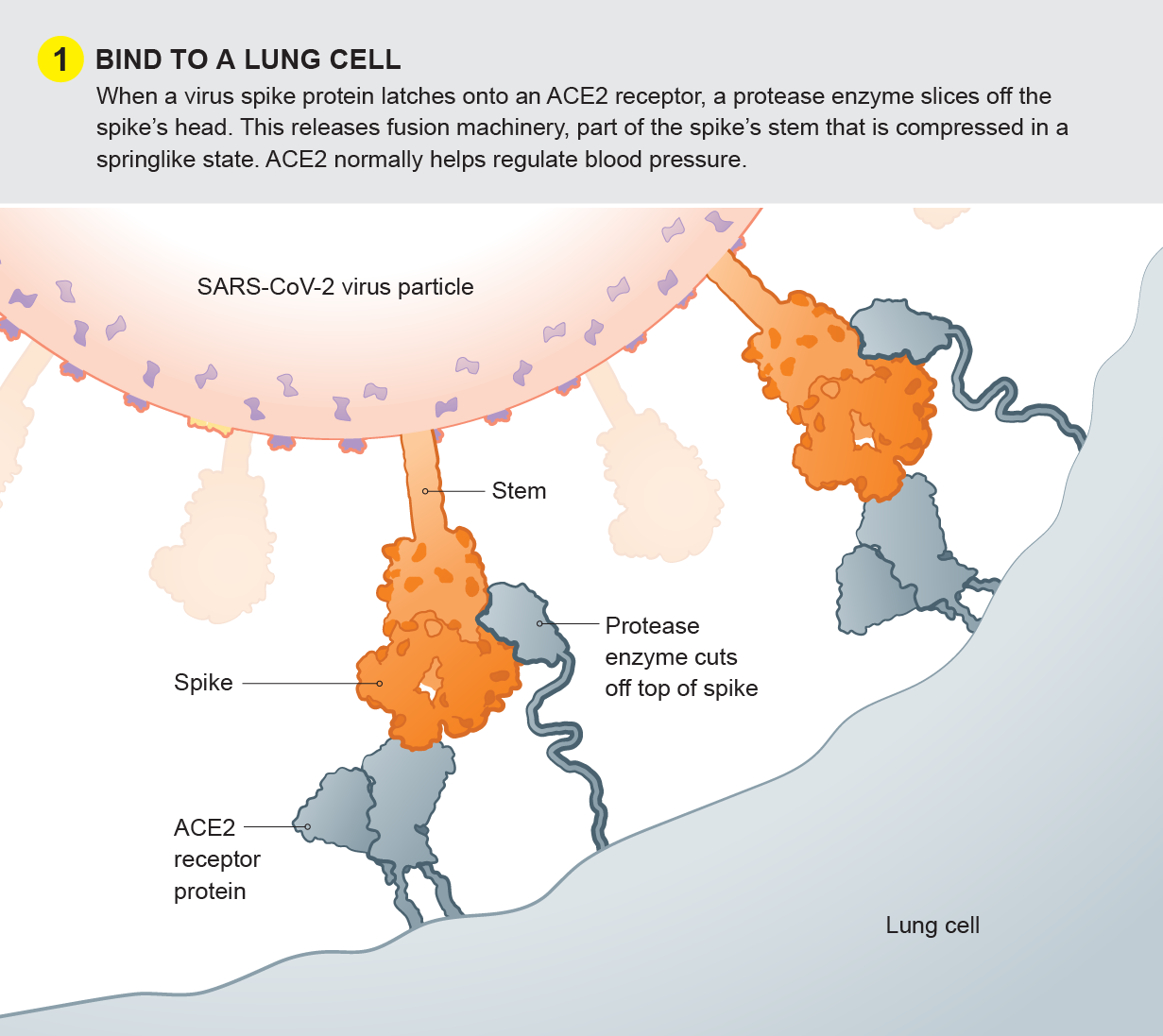
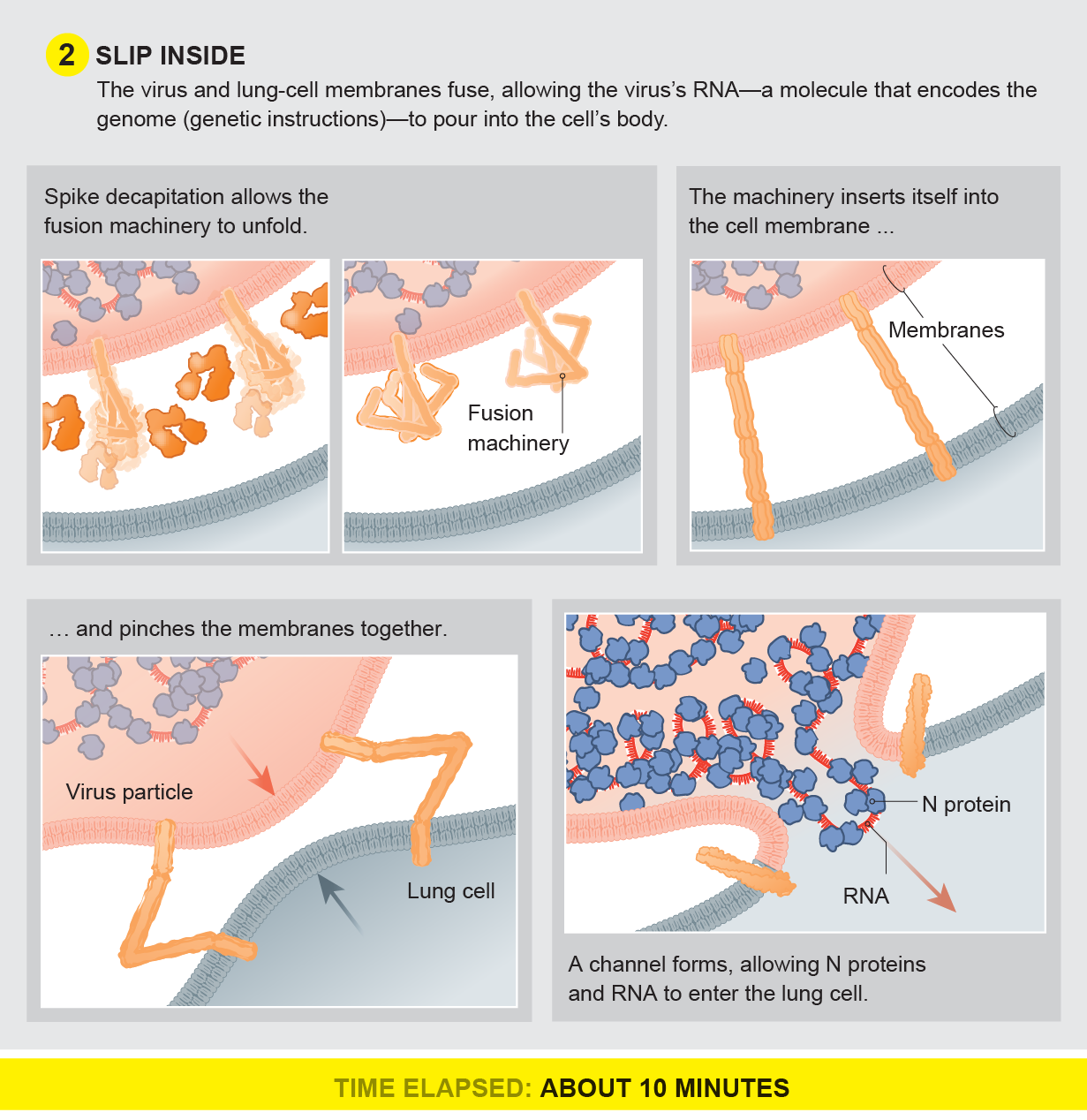
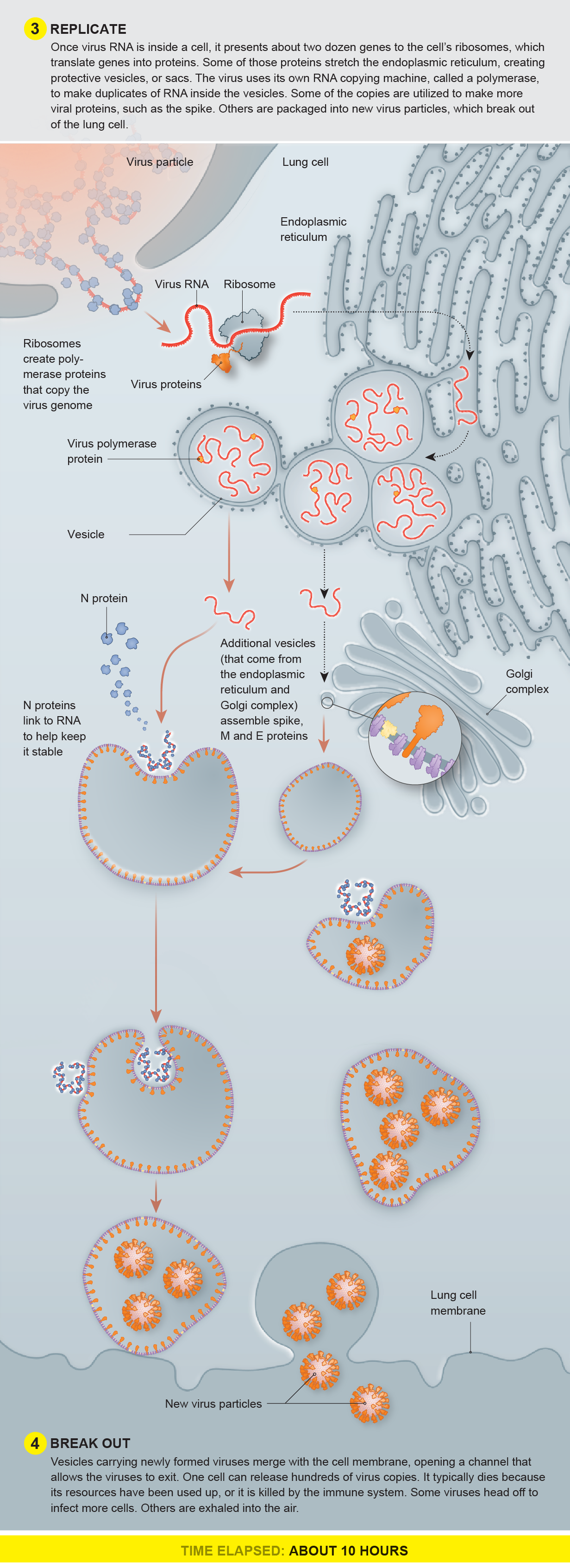
A SARS-CoV-2 particle enters a person’s nose or mouth and floats in the airway until it brushes against a lung cell that has an ACE2 receptor on the surface. The virus binds to that cell, slips inside and uses the cell’s machinery to help make copies of itself. They break out, leaving the cell for dead, and penetrate other cells. Infected cells send out alarms to the immune system to try to neutralize or destroy the pathogens, but the viruses can prevent or intercept the signals, buying time to replicate widely before a person shows symptoms.
Drug and Vaccine Intervention
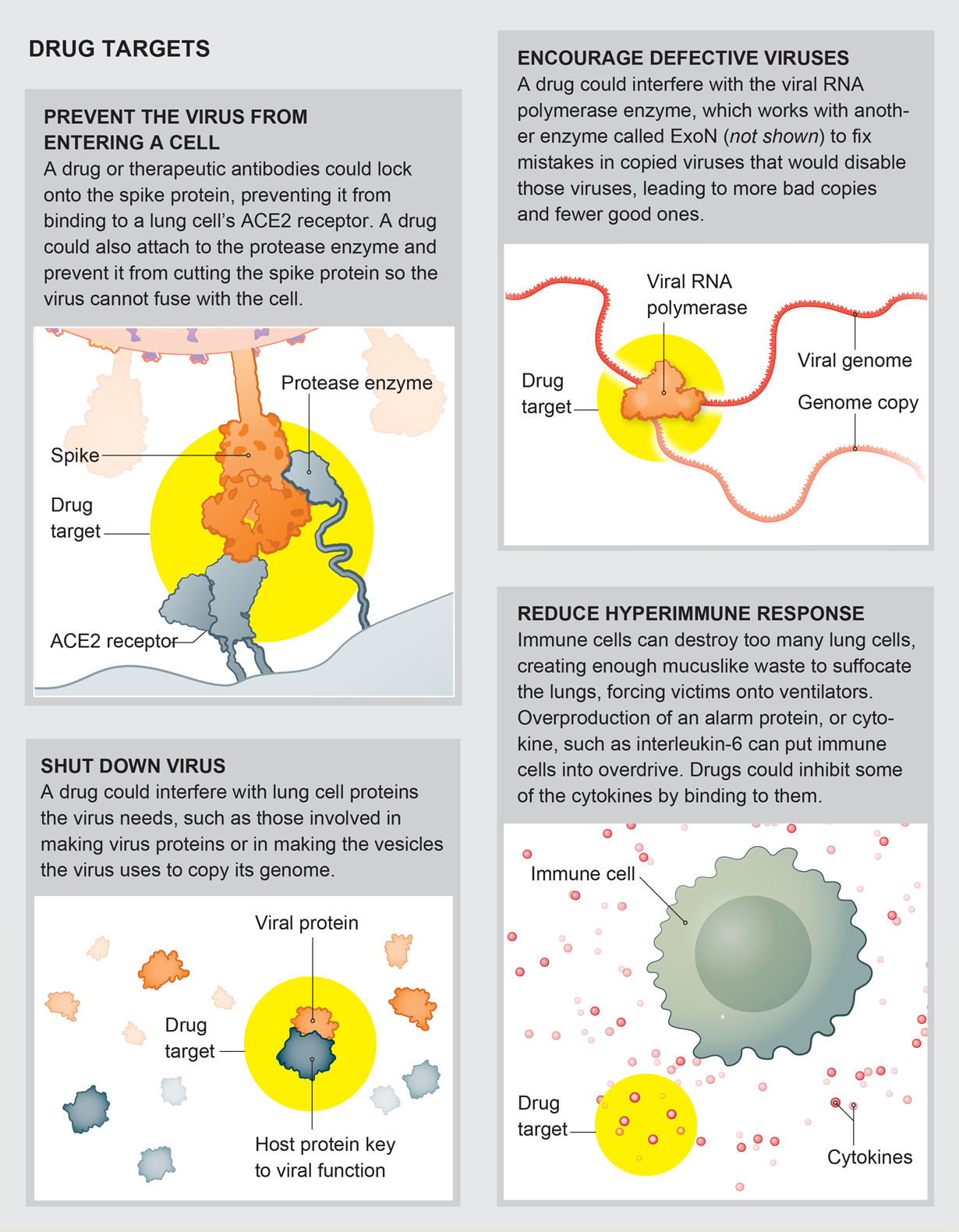
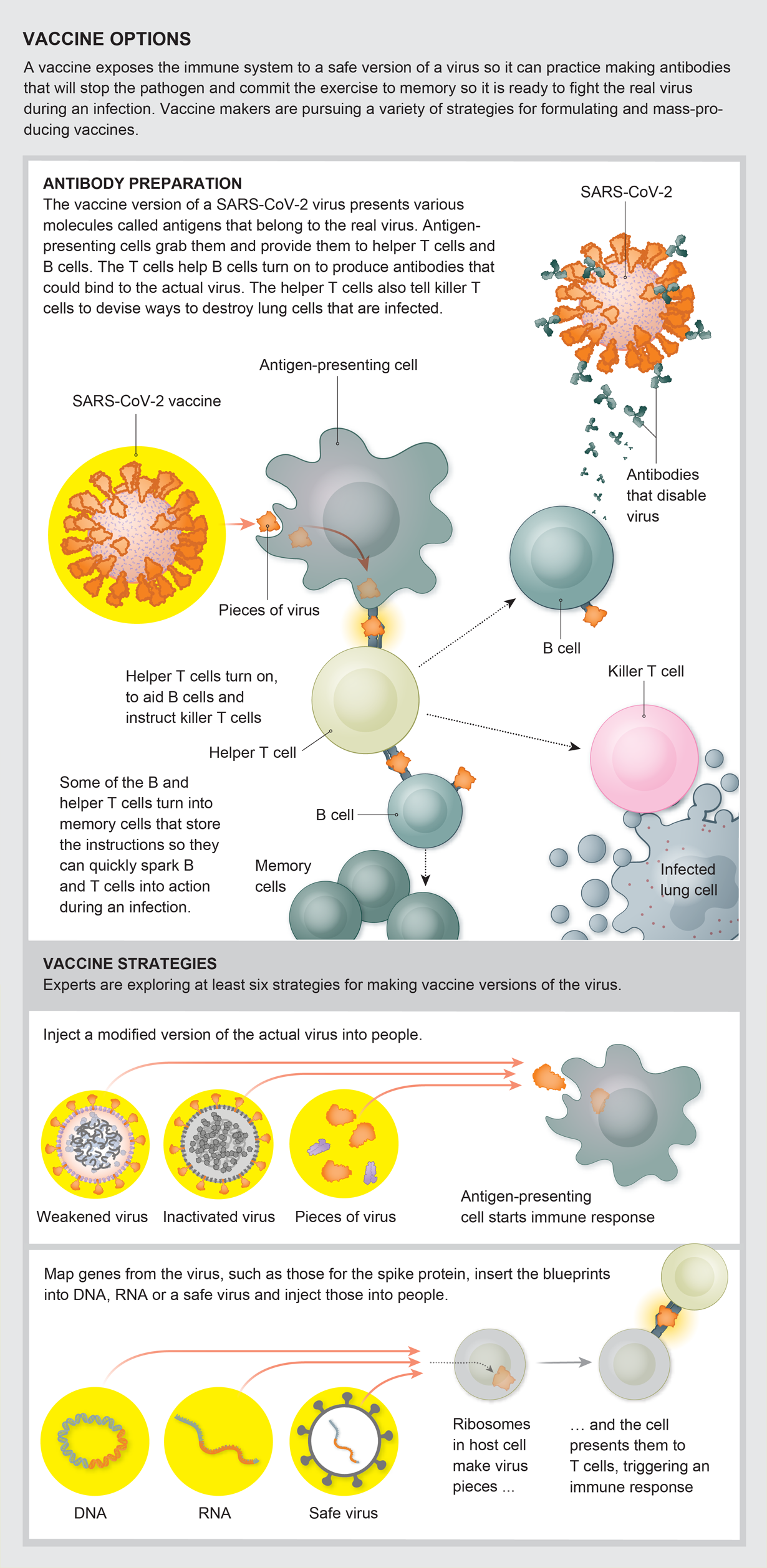
Commercial and university labs are investigating well over 100 drugs to fight COVID-19, the disease the SARS-CoV-2 virus causes. Most drugs would not destroy the virus directly but would interfere with it enough to allow the body’s immune system to clear the infection. Antiviral drugs generally stop a virus from attaching to a lung cell, prevent a virus from reproducing if it does invade a cell, or dampen an overreaction by the immune system, which can cause severe symptoms in infected people. Vaccines prepare the immune system to quickly and effectively fight a future infection.
The Remarkable and Mysterious coronavirus genome
The SARS-CoV-2 genome is a strand of RNA that is about 29,900 bases long—near the limit for RNA viruses. Influenza has about 13,500 bases, and the rhinoviruses that cause common colds have about 8,000. (A base is a pair of compounds that are the building blocks of RNA and DNA.) Because the genome is so large, many mutations could occur during replication that would cripple the virus, but SARS-CoV-2 can proofread and correct copies. This quality control is common in human cells and in DNA viruses but highly unusual in RNA viruses. The long genome also has accessory genes, not fully understood, some of which may help it fend off our immune system.
Read more about the coronavirus outbreak from Scientific American here. And read coverage from our international network of magazines here.