Perhaps the most unnerving aspect of COVID-19 is its startling range of severity: from completely asymptomatic to deadly. Starting early in the pandemic, researchers identified factors that put people at risk of a serious case of the disease, such as advanced age, having certain chronic diseases and being male. But these demographic trends do not get at the biological mechanisms that actually cause a life-threatening infection. Nor do they explain why some young, fit, healthy people become mortally ill from the SARS-CoV-2 virus.
Two related papers published in Science onSeptember 24 begin to address these mysteries. They may also partially account for men’s greater vulnerability to the virus and point the way to possible treatments and protective measures. Both studies highlight the critical role of a class of immune system proteins called interferons, so named because they interfere with the replication of viruses.
The new papers were produced by the COVID Human Genetic Effort, a huge international consortium of researchers hunting for genetic mutations that either make individuals unusually susceptible to SARS-CoV-2 or confer exceptional resistance. The consortium is co-led by Jean-Laurent Casanova of the Rockefeller University and Helen Su of the National Institute of Allergy and Infectious Diseases, who are co-senior authors of both of the studies.
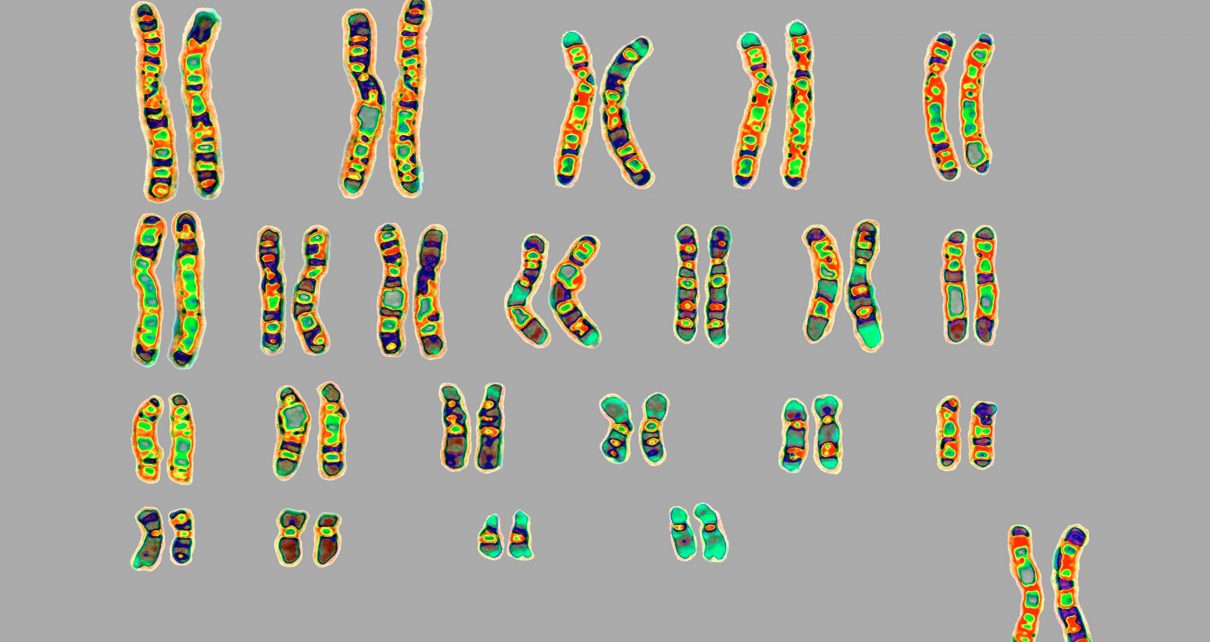
In their first paper, the researchers compared DNA from 659 gravely ill COVID-19 patients from around the world with DNA from a control group of 534 infected people who were only mildly affected by the novel coronavirus or did not have symptoms. The scientists specifically looked for mutations that would impair the production of type I interferons—a set of proteins made by every cell in the body that comprise a first-line defense against viruses. Previous work by Casanova and others showed that such mutations left people extremely vulnerable to influenza and other viruses. As it turned out, some of the same mutations associated with life-threatening flu were also present in 3.5 percent of patients with life-threatening COVID-19. No one in the new study’s control group had these mutations.
The second paper focuses on another mechanism that disables interferon responses in patients with severe COVID-19. In this set of studies, researchers examined blood samples from 987 such individuals and discovered that 13.7 percent contained antibodies—dubbed “auto-antibodies”—to the patients’ own type I interferons. In 10.2 percent of the subjects, the auto-antibodies completely blocked the action of these critical virus fighters.
Lab experiments showed that when human cells were exposed to plasma (the liquid part of blood) taken from patients with these self-attacking antibodies, the cells could not defend themselves against SARS-CoV-2. The antibodies were found in 12.5 percent of the severely ill men but only 2.6 percent of similarly ill women—making them a possible factor in the higher COVID-19 mortality rate among men. They were also more common in patients older than 65.
Antibodies to the body’s own cytokines, cell-signaling proteins of the immune system that include interferons, have been known to exacerbate other types of infections. The effect is the same as having a mutation that disrupts the production of that cytokine. “For example, if you have a mutation in gamma interferon or you have auto-antibodies against gamma interferon, which is a type II interferon, then you are prone to tuberculosis and related mycobacterial diseases,” Casanova says.
Still, he was stunned to find that the auto-antibodies were so prevalent among desperately ill COVID-19 patients, especially because they appear to be vanishingly rare in the general population. The researchers screened the blood of 1,227 healthy individuals and found only four (0.3 percent) with the auto-antibodies.
The finding that more than 10 percent of COVID-19 patients in the world’s intensive care units could have these antibodies “was beyond my wildest expectation,” Casanova says. Taken together, genetic and immunologic disabling of type I interferons could account for nearly 14 percent of life-threatening cases.
“The two papers are remarkable on multiple levels,” says Eleanor Fish, a professor of immunology at the University of Toronto, who studies interferons and was not involved in those new studies. “One is that they identified so quickly what is going on in life-threatening cases in the context of interferon response.” She notes that there was already growing evidence that interferons are important in clearing the virus, but data also indicate that SARS-CoV-2 is particularly adept at blocking the body’s interferon response.
“What these papers are showing is that while interferon may be suppressed [by SARS-CoV-2], it still confers protection against the virus,” says Elina Zúñiga, a professor of molecular biology at the University of California, San Diego, who was not involved with the studies. Zúñiga, who investigates immune responses to viruses, finds it especially “mind-blowing” that antibodies to interferons were discovered in so many patients. “Who would have thought that this would be one reason why patients can have more severe COVID-19?” she says.
A study by Dutch scientists, published in July in JAMA, supports the new genetics findings. The researchers describe two unrelated pairs of previously healthy, young brothers—with an average age of 26—who became desperately ill with COVID-19 and turned out to have a genetic mutation on their X chromosome that impaired interferon response.
If confirmed by further research, the new papers—along with previous work on interferons—have a number of implications for screening patients and treating severe COVID-19. The authors suggest that newly infected patients could be screened for the auto-antibodies with an inexpensive blood test to determine if they are at risk of a life-threatening case.
Because most of these antibodies appear to be directed at a type of interferon called interferon-alpha, Fish offers that such patients might respond well to treatment with interferon-beta. The latter protein plays a similar role in battling viral infections but would likely not be targeted by the antibodies.
Screening for these antibodies in the population as a whole might also be possible in countries with the resources to manage it, Zúñiga suggests. “For young people who think they are not much at risk, if they have these auto-antibodies, it might change their behavior,” she says. When a vaccine becomes available, Zúñiga adds, “there’s a rational argument to prioritize people who have these auto-antibodies.”
Perhaps the most immediate implication of the new studies concerns the use of convalescent plasma, an experimental treatment made from the blood of people who have recovered from COVID-19. In August the U.S. Food and Drug Administration issued a controversial “emergency use authorization” for the blood product. Zúñiga points out that it would be important to screen plasma donors for auto-antibodies. “If you have severe COVID-19, would you like to receive antibodies that neutralize an antiviral response?” she asks. “No thank you.”
Given the growing evidence that interferon plays a crucial role in arresting severe infection, Fish believes that treating COVID-19 patients with interferon, regardless of their antibody or genetic status, could be a winning tactic, particularly early in the infection. She points to exploratory studies on interferon in Cuba and Wuhan, China, that showed promising effects on mortality rates and earlier clearance of the virus.
But determining the timing and other details of such treatment will be vital. “Interferon can be a double-edged sword in many infections,” Zúñiga says. “It activates many immune cells, but it can enhance inflammation as well. And it can have a negative immunoregulatory role, activating factors that suppress the immune response.”
Experts seem to agree that interferons would have to be given early to help shut down the infection. Once a patient develops an extreme immune reaction sometimes called a “cytokine storm,” interferons are unlikely to be of use, Fish says.
Dozens of COVID-19 clinical trials are already underway to test the efficacy of various types of interferon therapies, which can be given as a nasal spray or injection. One large study, conducted by the National Institute of Allergy and Infectious Diseases, is comparing the antiviral remdesivir alone with a combined therapy of the drug and interferon-beta. And Fish is involved in a study in Santiago, Chile, that will investigate whether giving interferons to members of a household where someone has been infected with the coronavirus could prevent them from falling ill. It remains to be seen whether any of these therapies pan out, but the new findings at least unlock one more piece of the COVID-19 puzzle.
Read more about the coronavirus outbreak from Scientific American here. And read coverage from our international network of magazines here.