The unequal impact of COVID-19 on the health of certain groups, including Black, Latinx and Native Americans, became clear from the outset of the pandemic. The Navajo Nation, Diné Bikéyah, made headlines throughout May 2020 when its per capita COVID-19 infection rate surpassed that of every U.S. state.
But although COVID-19’s rates in Canada have been high in the Black community, and in neighborhoods where there are large populations of people of color, its prevalence to date among Indigenous people in Canada has been less than one quarter that of non-Indigenous Canadians, with a third of the fatalities and a 30 percent higher recovery rate.
The ability of First Nations, Inuit and Métis communities in Canada to prevail during the pandemic was largely rooted in their shaping their own public health strategies after confronting the toll wrought by previous disease outbreaks and long-running neglect by health authorities.
Health care among Indigenous nations in Canada has always faced hardships shaped by social and structural inequities in housing and poverty and other social determinants—“the conditions in which people are born, grow, live, work and age,” as defined by the World Health Organization. Staging an effective public health response during the ongoing pandemic has required that these communities regain control and oversight over prevention and treatment measures in their own localities. Indigenous people across Turtle Island, the land now known as North America, share the fundamental right to self-determination over all activities related to their lives and well-being, as articulated by the 2007 United Nations Declaration on the Rights of Indigenous Peoples.
Colonization by European settlers not only took away the autonomy of Indigenous communities but used medicine and public health as tools to do so. In Indigenous communities across North America and in Australia, public health practices that dealt with the infections that settlers brought with them often turned into a pretext for imposing social control measures.Quarantine established the “clean” perimeters of community and determined which activities were allowed and which would be excluded during an outbreak. Local Indigenous healing practices were stifled or banned. Indigenous knowledge of medicine and healing was ignored, and people were depicted as primitive, childish and dirty. Across Canada, Indigenous people were relocated outside of their communities for treatment and segregated into “Indian Hospitals.” These paternalistic and racist attitudes and actions diminished Indigenous rights and sovereignty.
Historical practices of medicine and public health continue to affect the way that Indigenous communities view health care. A study of people with tuberculosis in Nunavut, for example, found that previous experiences with public health approaches to treating tuberculosis in the 1950s continue to deter some Inuit from seeking treatment for that disease. One study participant described feelings of lack of respect and autonomy that affected their attitudes toward adherence to public health recommendations: “Health care people do not treat patients with respect. It is as if they don’t care to explain anything, like the patients won’t understand anyway and the health care people know better. People are generally not told about things. They are not informed so that they can have a choice. The doctors or nurses choose for them.”
In addition to eroding trust and disrupting access to traditional healing, colonization underpins ongoing inequities in social determinants of health like housing, poverty and food security, which can expose Indigenous people to a higher risk of both contracting COVID-19 and developing a severe infection. Thirty percent of homes in the Navajo Nation do not have access to running water, making hand hygiene recommendations almost impossible to follow. Obesity and type 2 diabetes—conditions related, in part, to access to healthy, affordable food—are also more common and lead to an increased risk of severe outcomes from infectious disease. Lastly, access to high-quality care is limited by the chronic underfunding of the Indian Health Service (IHS), part of the Department and Health and Human Services, that provides care for all federally recognized tribe members in the U.S. The IHS budgets $4,078 per capita, compared to $13,185 per Medicare beneficiary. According to data from 2018, 25 percent of positions for physicians, nurses and other providers within the IHS remained vacant.
In many instances, similar structural inequities have undermined the ability to enact public health recommendations in many First Nations, Inuit and Métis communities in Canada. Inadequate infrastructure contributed to severe disparities in the rates of infection between Indigenous and non-Indigenous people during the H1N1 flu pandemic of 2009. But during the current pandemic, knowledge gained from the H1N1 outbreak, as well as the advance warning of the arrival of COVID-19, impelled Indigenous leaders to immediately close their borders and update emergency response plans, knowing that once COVID-19 entered their communities, it would spread rapidly.
COVID-19 was able to penetrate deeply into the Navajo Nation, but, once it did, leaders reacted swiftly to secure funding for personal protective equipment, water stations, food delivery and access to testing. Members of the Navajo community of all ages demonstrated generosity, resourcefulness, collaboration and resilience in organizing and delivering support. As Heather Kovich, a physician working with the Indian Health Service, describes: “But where cell-phone service is spotty and broadband nonexistent, human networks are strong and extensive.” This grassroots response illustrates the centrality of community as a component of resilience and wellness, an idea interlaced through many Indigenous nations. While rates of COVID-19 continued to climb in many states, they stabilized in the Navajo Nation, despite the initial high rates, and despite limited infrastructure to support health and wellness.
The border closure and community-based response to COVID-19 uphold the principle of self-determination in which Indigenous peoples have a right to determine their own paths to healing and health for their communities. Other examples include the innovative educational materials and public health campaigns that have been created by many diverse Indigenous communities. These materials build on prevention, isolation and containment measures put forward by public health institutions, but are grounded in the local context of the various nations, and their language, culture, physical and social environment.
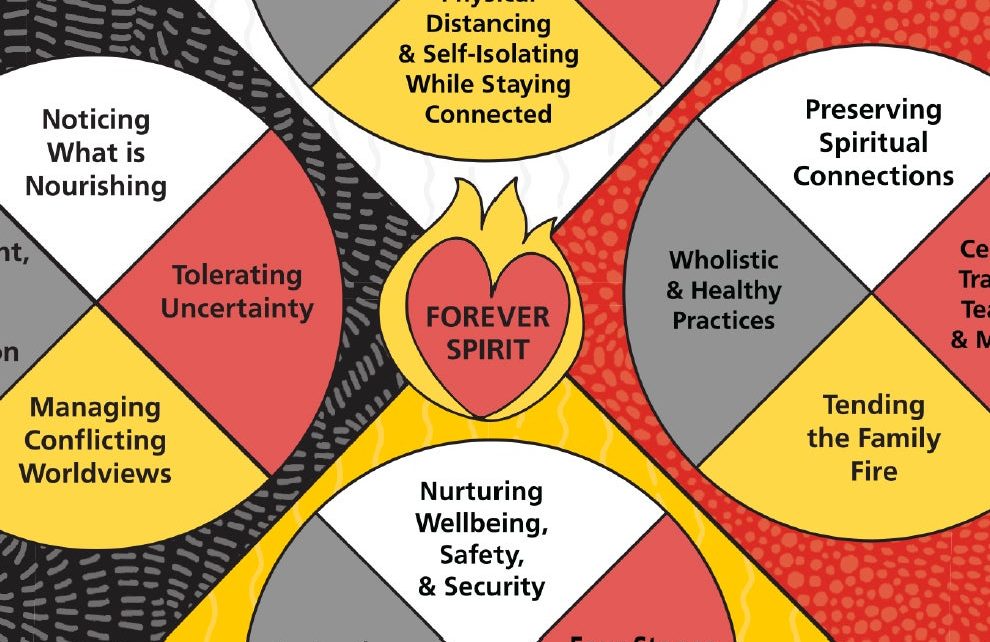
One beautiful example that draws on the wisdom of elders and knowledge keepers is in adapting the Four Directions Medicine Wheel, a framework that encompasses multiple dimensions of well-being beyond the focus on physical and mental health in biomedical models of care. The Center for Wise Practices in Indigenous Health at Women’s College Hospital in Toronto, Canada, created a medicine wheel dedicated to purveying a holistic approach to disease prevention and building physical, emotional, mental and spiritual resilience during the pandemic. It counsels handwashing, disinfecting, managing conflicting worldviews, protecting elders and youth and preserving spiritual connections.
Another clear example of self-determination in response to COVID-19 is an initiative begun during the pandemic to collect Indigenous-specific data on disease incidence. It is combined with legal agreements that protect personal information and guarantee control, ownership and possession of data in various Indigenous communities across the globe
Despite the diversity of Indigenous nations across Turtle Island, resilience and commitment to community well-being in the face of the unprecedented impacts of COVID-19 are shared values. We cannot always insulate our communities from the spread of COVID-19, nor can we always mitigate the lack of investment for years in social determinants of health by local and federal governments. However, COVID-19 has demonstrated that the sovereignty, leadership and knowledge of Indigenous nations is an essential foundation for public health during moments of crisis.
This essay was adapted from a commentary in the Sept. 21, 2020 edition of CMAJ, published by the Canadian Medical Association, entitled “COVID-19 and the Decolonization of Indigenous Public Health.”