A viral outbreak has killed more than 6,500 children in the Democratic Republic of the Congo (DRC) and is still spreading through the country. The foe isn’t the feared coronavirus, which has only just reached the DRC. It’s an old, familiar and underestimated adversary: measles.
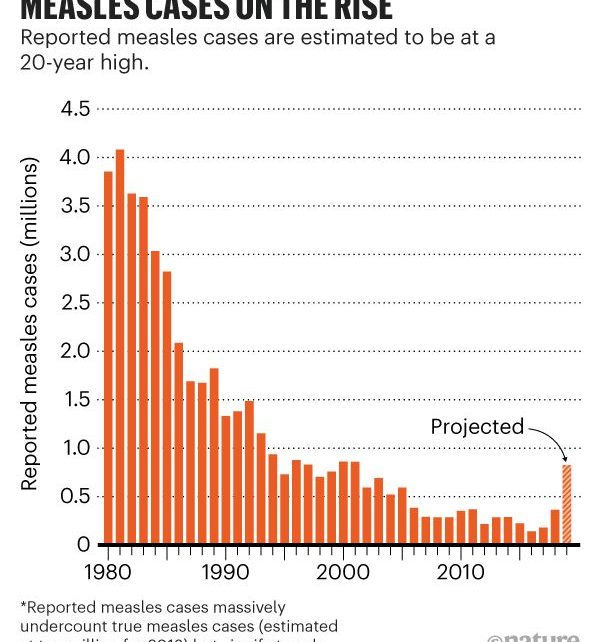
Cases began to spike here in October 2018. Children became weak, feverish and congested, with red eyes and painful sores in their mouths, all with the telltale rash of measles. “We have been running after the virus ever since,” says Balcha Masresha, an epidemiologist with the World Health Organization (WHO) regional Africa office in Brazzaville in the neighbouring Republic of Congo. The situation has mushroomed into what WHO experts say might be the largest documented measles outbreak in one country since the world gained a measles vaccine in 1963 (see ‘Measles cases on the rise’).
The highly contagious measles virus continues to spread around the globe. In 2018, cases surged to an estimated 10 million worldwide, with 140,000 deaths, a 58% increase since 2016. In rich countries, scattered measles outbreaks are fuelled by people refusing to vaccinate their children. But in poor countries, the problems are health systems so broken and underfunded that it is nigh-on impossible to deliver the vaccine to people who need it. The DRC’s flood of cases shows why measles will keep flaring up despite efforts to control it. And the situation will only worsen with the COVID-19 pandemic: more than 20 countries have already suspended measles vaccination campaigns as healthcare workers scramble to deal with coronavirus.
The other deadly virus
In poor countries, measles is a killer, especially in combination with malnutrition and vitamin A deficiency. Estimates are uncertain, but the death rate in developing countries hovers around 3–6%, and it can spike as high as 30% in the worst outbreaks, according to the WHO. Its victims often die of complications including pneumonia or diarrhoea and dehydration. Those who recover can be left with permanent disabilities, including blindness, hearing loss and brain damage. The virus also impairs the immune system for months or years after infection, creating “immune amnesia” that leaves children vulnerable to other infections.
The virus is so contagious that few unvaccinated people who come into contact with it are spared its effects. Scientists define infectiousness using the ‘reproduction number’—how many people, on average, would be infected by a single person with the virus, in a population that has no immunity. For Ebola, that number is estimated at 1.5–2.5. The new coronavirus terrifying the world seems to be somewhere between 2 and 3. Measles tops the charts with a reproduction number of 12–18, which makes it the most contagious virus known. You don’t need to be in the same room as an infected person to catch the virus—it is spread by respiratory droplets that can linger in the air for hours.
Two doses of a safe and effective vaccine can prevent measles; one dose provides partial protection. Many children in poor countries are lucky to get a single dose. Because the virus is so contagious, 92–95% of a population needs to be fully immunized to ward off outbreaks. In the DRC, only 57% of children received even one dose of measles vaccine in 2018, according to a UNICEF study, creating ideal conditions for the virus to explode.
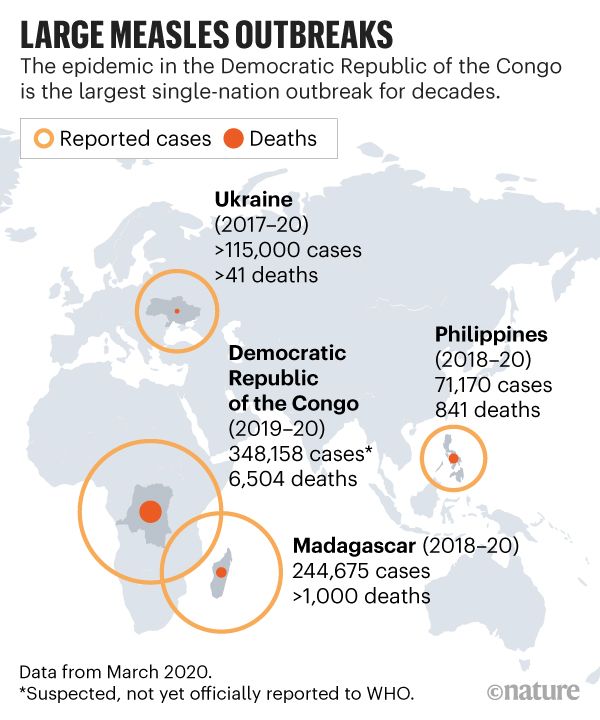
In other countries, too, measles is a constant, simmering at low levels until the number of children susceptible to the virus builds up and it takes off (see ‘Large measles outbreaks’). “Pretty much name any country and you will find measles there,” says Robb Linkins, a measles specialist in the global immunization division at the US Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia, and chair of the Measles & Rubella Initiative, a partnership of five organizations.
In each region, a slightly different mix of factors leads to an outbreak.
In Madagascar, a shortage of measles vaccine helped fuel an outbreak that has swept the island nation starting in 2018, causing more than 240,000 cases and 1,000 deaths.
And in Ukraine, after a child died of unrelated causes following a measles jab in 2008, vaccination coverage plummeted from 95% that year to 31% in 2016, says Linkins. He says no one was surprised when, in 2017, a huge outbreak hit that has led to more than 115,000 cases.
Failure modes
The DRC has difficulties on a number of levels. The country has such a high birth rate—3.5 million children are born each year—that it needs to conduct mass vaccination campaigns every two years. Those campaigns, in which tens of thousands of health workers fan out across this vast country, are a logistical nightmare. First, the government has to get the vaccine from the capital, Kinshasa, to remote villages that can be reached only by helicopter—or through bloody conflict zones in the eastern part of the country.
The vaccine must be kept between 2 °C and 8 °C from the time it leaves the warehouse until it is administered—a challenge in a tropical environment where power outages are frequent. Health workers must be trained to inject it safely, a much more difficult task than dropping liquid polio vaccine on a child’s tongue. The vaccine comes as a powder, which must be reconstituted with an accompanying solution of sterile diluent and then used within 6 hours. It also comes in ten-dose vials; worried about wastage, vaccinators are sometimes hesitant to open one when just a few children show up to a session, so the children go unimmunized.
On top of that, clinics have to be open when parents can make it, and vaccinators have to be paid or they won’t come, either—a problem in a country plagued with corruption.
Health workers are stretched thin at the best of times, and the DRC has been battling Ebola, outbreaks of cholera and yellow fever—and now the coronavirus. And measles is such a constant that it often takes lower priority than other diseases. In addition to these outbreaks, “DRC is confronted not only with political challenges but a long-running civil war,” says Katrina Kretsinger, a medical epidemiologist and global measles expert at the WHO in Geneva, Switzerland. “When in a firefighting mode, it is hard to sit back and say, ‘Here is the long-term view of what needs to happen’” with measles, she says.
Money is a major problem. Vaccination campaigns cost around US$1.80 per child in the DRC, says Masresha; international donors foot some of the bill, but the country is expected to pay a share. In 2010, the DRC couldn’t muster the funds and cancelled a scheduled campaign. An outbreak that hit at the end of the year raged for more than 30 months. Further campaigns in 2013–14 and 2016–17 didn’t reach enough children. In June 2019, after cases soared to more than 3,500 a week at the start of the year, the DRC government declared an epidemic, opening the door to further international aid. By the end of the year, 18.5 million children had been vaccinated.
The WHO estimates that there have been more than 348,000 cases and 6,500 deaths, but Francisco Luquero, an epidemiologist at Epicentre, the research arm of Médecins Sans Frontières (MSF, also called Doctors Without Borders) in Paris, thinks the outbreak is much worse. The case count reflects only people who go to health centres, he says; many don’t in the DRC. As for the mortality estimates, “they count deaths that happen right after a measles case. They should look out for the next five years,” he says, because of immune amnesia. “The outbreak will have a profound impact on public health.”
Eradication hopes
Steve Cochi, a paediatrician and senior adviser to the CDC’s global-immunization division, is especially frustrated by measles’s global toll, because from a biological and technical standpoint, he says, the disease could be eradicated. Unlike Ebola, yellow fever or (probably) the new coronavirus, it has no animal host, and a cheap and effective vaccine exists.
A new vaccine delivery system being developed by two teams—one a collaboration between the CDC and the Georgia Institute of Technology and Micron Biomedical, both in Atlanta, and the other at Vaxxas, a biotech company based in Sydney, Australia—could be a “game changer” for measles control and elimination, says Cochi, who is a fierce advocate of global eradication. The vaccine uses a technology called a microarray patch, which looks like a small round bandage with hundreds of microneedles, each carrying a small amount of live, freeze-dried vaccine. Applied with a small push, it delivers vaccine under the skin in 5 minutes.
“It is very thermostable, takes up little space, doesn’t have to be reconstituted, and you don’t have to worry about safety,” Cochi says. But the measles patch has languished in development for lack of funding, he says, and has yet to reach clinical trials, although these are intended to begin by the end of 2020 or in early 2021. “It is totally frustrating,” he says.
Until polio is eradicated, the world does not have the appetite or the money to target another disease for extinction, Cochi says. Originally slated for completion in 2000, the polio eradication initiative has blasted through one deadline after another as frustrated donors have poured billions of dollars into reaching the ever-receding goal. No one wants a repeat performance.
In 2010, the WHO’s key Strategic Advisory Group of Experts on Immunization (SAGE) declared that measles can and should be eradicated, but it stopped short of recommending a target date. Since then, advocates have been lobbying the WHO to launch a global measles-eradication campaign and set a date for completion, as it did for smallpox and polio.
At a meeting last October, however, SAGE recommended a different tack: instead of setting eradication deadlines that would be difficult to meet, the group advised waiting until success is actually in sight—say, 5 years away—before pushing full-bore to wipe out the disease. Doing so would require boosting rates of routine immunization with two doses of measles vaccine to a level never achieved before. The DRC is one of about 20 countries that have yet to add the second dose to its regime. And even that wouldn’t be enough. Eradication would also depend on improving the quality of mass campaigns and bringing an improved vaccine into use. Those goals are very far away, measles experts say.
Coronavirus crunch
The coronavirus pandemic has dealt measles-control efforts another huge blow. On 26 March, SAGE recommended that countries temporarily suspend all preventive mass-vaccination campaigns, including those for measles. Already, 23 countries have suspended scheduled measles campaigns, and others will probably follow suit, says Linkins. This means that 78 million children will not be vaccinated as planned, he says. The DRC, however, is continuing its outbreak response.
“We must protect vulnerable populations from the spread of COVID-19,” Linkins says, but limiting measles-immunization activities will create “dangerous immunity gaps”. Modellers are just beginning work to estimate the impact of COVID-19 on measles control, but it is clear that countries must be able to resume their campaigns quickly after the pandemic subsides, he says.
With campaigns cancelled and global measles-immunization rates for just one dose of vaccine stalled at 86%, the unrelenting cycle of outbreaks will continue. This DRC outbreak will subside, but Masresha says it will be a “temporary victory”: the virus will rebound.
This article is reproduced with permission and was first published on April 7 2020.
Read more about the coronavirus outbreak here.