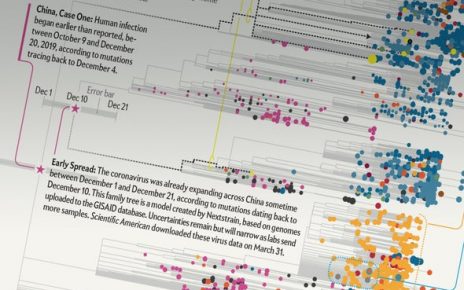
COVID-19 is different from the viral epidemics of the recent past in a few ways: it is more widespread than severe acute respiratory syndrome, more infectious than seasonal influenza and has killed more people than Ebola.
And it is different in the way that epidemiologists are tracking its progress. Instead of relying principally on the number of infections, or the ratio of deaths to infections—known as the case fatality rate—researchers are looking at the daily deaths attributed to COVID-19 to monitor the impact of the disease and to guide responses.
In part, that’s due to a lack of testing in many countries—and the virus’s ability to spread in people who don’t show symptoms—both of which make counting the number of infections very difficult. COVID-19 has also been more fatal than many recent epidemics, which makes its death toll relevant to understanding the pandemic more broadly.
As of early April, more than a million coronavirus cases had been reported around the world. There have been more than 80,000 deaths reported so far, with Italy, the United States and Spain reporting the highest numbers. And the pandemic has yet to hit its stride in most low- and middle-income countries, where it could cause much more damage. “This is a virus with a considerable lethal potential,” says Sheila Bird, a biostatistician at the University of Cambridge, UK.
COVID-19 is not deadly to most people: the World Health Organization estimates that it is fatal in about 3.4% of reported cases, and the risk of death varies by age group and a host of other factors. But the pandemic is now widespread enough that the reported number of deaths within a country, day by day or week by week, is a surer tracker of the disease’s progress and effectiveness of containment than are other measures. When the rate of new deaths per day starts to slow or reduces, it’s a good sign that the disease has peaked, and several countries are seeing early signs that this is happening (see ‘Counting Deaths’). The rates can also be used to predict health-care needs.
Deathly models
As the virus’s spread started to gain momentum in the United States, a team at the University of Washington in Seattle used the daily death rates in a model to predict the number of beds and ventilators that US hospitals would need. “Our modeling approach is based off the deaths—that is the core part that tells us about the epidemic,” says Theo Vos, an epidemiologist at the Institute for Health Metrics and Evaluation (IHME) at the university. IHME’s projections were reportedly among those used by US President Donald Trump’s administration in late March just before announcing stricter control measures in the country.
But tracking death rates is hardly straightforward. In the United States, there are reports that cases are being undercounted for a variety of reasons. . And there will be delays in national death tallies as hospitals and nursing homes gather their numbers. Delays in testing can be accounted for statistically, says Bird. And undercounting may be managed, too, at least within a region. “If the relative proportion of undercounted deaths remains constant over time, the effect would be that the shape of the curve does not change,” Vos says. This would not determine the true number of deaths due to COVID-19, but would accurately predict the peak and end of the epidemic, he adds.
There are also limitations to comparing trends between countries. When Italy’s counts began to soar in mid-March, there were questions about the comparatively low number of deaths in Germany, which numbered about a dozen at the time. Italy’s high death toll might be affected by the fact that much of the country’s population is more than 65 years old, says Graziano Onder, a gerontologist at the Italian National Institute of Health, a public-health and research centre in Rome, where he has been tallying the country’s deaths.
Italy’s definition of a ‘coronavirus death’ could also contribute to its high numbers. Medics there count anyone who tested positive for the virus when they died, regardless of pre-existing diseases that may have contributed. And some have pointed to a combination of extensive testing and early action in Germany as the reason for the disparity.
Preparing for the onslaught
The United States is now seeing a shortage of protective gear in hospitals, and a ventilator shortage. And in low- and middle-income countries, many deaths are likely to go uncounted because they happen in the home.
Capturing the daily death toll will continue to challenge epidemiologists, says Prabhat Jha, an epidemiologist at the Dalla Lana School of Public Health at the University of Toronto, Canada. But there are tools available to estimate this important rate, such as examining how many more people died on a particular day, compared to that day in a previous month or year. Jha has also pioneered ‘verbal autopsies’, in which health workers interview family members of a random sample of people who have died to ascertain the cause of death. In preparation for the coronavirus, Jha says he’s contacted the government of India to resurrect such efforts. “We’ve suggested to the registrar general to get those teams out now.”
Although figures might not always be comparable, more approaches to counting the dead are useful. Diseases have always cut differing paths through communities, says Maia Majumder, an epidemiologist at Harvard Medical School and Boston Children’s Hospital in Massachusetts. “This disease is going to look enormously different from one context to another, and we need to get comfortable with that,” says Majumder.
This article is reproduced with permission and was first published on April 9 2020.
Read more about the coronavirus outbreak here.